How Do People Not Know They Are Pregnant Domain_10
If You Are Pregnant: Information on fetal development, abortion and alternatives
- Printable versions:
- English version (PDF)
- Versión Española - Spanish version (PDF)
Resources used by the Minnesota Department of Health for this publication are Human Embryology and Developmental Biology, Fifth Edition, 2014; Larsen's Human Embryology, Fifth Edition, 2014; The Developing Human, 10th Edition, 2016; and In the Womb, 2006.
The photographs in this booklet are credited to Lennart Nilsson/TT Images and are used by permission; except for week 38 copyright Minnesota Department of Health.
The illustrations found throughout this booklet were created by Peg Gerrity, Houston, Texas. Copyright.
August 2019
Introduction
The information provided in this booklet is designed to provide you with basic, medically accurate information on the fetal development of your unborn child in two-week intervals from conception to birth. It will include such details as average weight and length, organ development and movement for that age.
This booklet also includes information on the methods of abortion, as well as the medical risks associated with abortion. In addition, the possible emotional side effects of abortion, the possibility of fetal pain, and some common medical risks associated with carrying a fetus to term are discussed.
If You Are Pregnant: Information on Fetal Development, Abortion and Alternatives presents current, medically reliable information. However, each woman and unborn fetus are unique. When considering an abortion, a woman should talk to her doctor about the procedures and alternatives before committing to or paying for an abortion. It is a woman's right to be fully informed about the procedures, complications and risks involved in an abortion. It is a doctor's legal responsibility to provide that information. Additionally, the law requires that your doctor must tell you how old your unborn child is and must give you an opportunity to ask questions.
A directory of services is also available. By calling or visiting the agencies and offices in the directory you can find out about alternatives to abortion, obtain assistance in making an adoption plan for your baby; and locate public and private agencies that offer medical and financial help during pregnancy, childbirth and while a child is dependent. The directory is available online: If You Are Pregnant: A Directory of Services Available in Minnesota. (PDF)
This document was developed by the Minnesota Department of Health in response to the 2003 legislative passage of the Woman's Right to Know Act. Minnesota laws related to abortion include:
Minnesota Statutes section 145.4241 - 145.4249
[Woman's Right to Know Act]
Minnesota Statutes section 145.423
[Abortion; Live Births]
Minnesota Statutes section 145.412
[Criminal Acts]
Minnesota Statutes section 144.343
[Pregnancy, Venereal Disease, Alcohol or Drug Abuse, Abortion]
Minnesota Statutes section 145.1621
[Disposition of Aborted or Miscarried Fetuses]
Your Legal Rights
You have a right to voluntary and informed consent before agreeing to an abortion. "Voluntary and informed consent" means the following information must be provided to you in person or over the phone by the abortion physician at least 24 hours prior to the abortion:
- Potential medical risks associated with the abortion procedure that will be used in your abortion, including risks of infection, hemorrhage, and danger to subsequent pregnancies and infertility
- Probable gestational age of the fetus at time of abortion
- Medical risks of carrying the fetus to term
You must be informed by the physician or his/her agent at least 24 hours prior to the abortion:
- That medical benefits may be available for prenatal care, childbirth and neonatal care
- That the father is liable to assist in the support of the child
- That you have the right to review the printed materials that describe the unborn fetus, the list of agencies that offer alternatives to abortion and information on fetal pain
The doctor must give you an opportunity to ask questions. You must certify in writing prior to the abortion that the above information has been furnished to you and that you have had an opportunity to review the printed materials.
If any of these provisions were not observed, you have the right to take legal action against the abortion provider for actual and punitive damages.
When a medical emergency compels the performance of an abortion, the doctor is required to inform you, prior to the abortion if possible, of the medical indications supporting the doctor's judgment that an abortion is necessary. An abortion may be necessary in a medical emergency to avert the death of the woman or because to delay 24 hours will create serious risk of substantial and irreversible impairment of a major bodily function of the woman.
Fetal Development
Conception (also called fertilization) occurs when a woman's egg is fertilized by a sperm penetrating it. At this moment an individual's unique set of DNA is created, captured in a single cell. Rapid development and growth begin. Within three to four days, the egg begins to develop rapidly. Within a few days the cluster of what is now 32 to 64 cells leaves the fallopian tube and moves into the uterus. This group of cells is now a hollow sphere called a blastocyst. By the eighth day after conception the blastocyst has begun to attach to (implant itself into) the wall of the uterus where it will grow at a rapid rate.
The term embryo refers to a developing human from implantation until the eighth week of pregnancy. After the eighth week, the unborn child is referred to as a fetus. Ages in this handbook are listed from both the estimated day of conception and from the first day of the last normal menstrual period. Lengths are measured from the top of the head to the rump.
A pregnant woman may notice her first missed menstrual period at the end of the second week after conception, or about four weeks after the first day of her last normal period. There are different kinds of tests for pregnancy. Some may not be accurate for up to three weeks after conception, or five weeks after the first day of the last normal period. The most accurate way to determine if you have a viable pregnancy and its length is by ultrasound.
First Trimester
Day 1
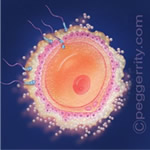 Approximately 2 weeks after the first day of the last normal menstrual period.
Approximately 2 weeks after the first day of the last normal menstrual period.
Conception, also known as fertilization, occurs when the egg from the woman unites with the sperm from the male, forming a single cell. At this moment, an individual's unique genetic material is created.
2 Weeks
4 weeks after the first day of the last normal menstrual period. (No illustration of 2 weeks is available.)
- The cells rapidly divide as they travel down the Fallopian tube.
- By day 7, the ball of cells, called a blastocyst, begins implanting into the woman's uterus.
- In the third week, a groove forms along most of the length of the embryo's back.
- The upper edges of the groove will fold over onto themselves, and begin to create a hollow tube.
- The embryo is about 1/10 of an inch long at this time.
4 Weeks
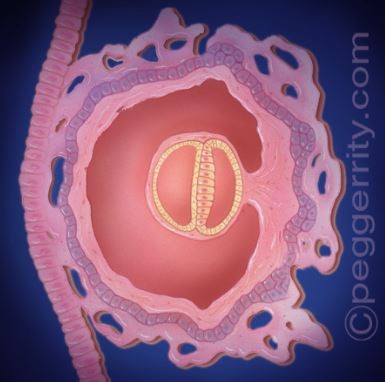 6 weeks after the first day of the last normal menstrual period.
6 weeks after the first day of the last normal menstrual period.
- The embryo is about 1/6 to 1/4 inch long.
- Structures that will become arms and legs, called limb buds, begin to appear.
- On day 22 or 23, the heart begins to beat. By the end of week 4, the heart is circulating primitive blood cells throughout the embryo.
- By the end of week 4, the edges of the groove have zipped together, forming a hollow tube. This is the neural tube, the beginnings of the brain and spinal cord.
6 Weeks
 8 weeks after the first day of the last normal menstrual period.
8 weeks after the first day of the last normal menstrual period.
- The embryo is about 1/2 to 3/4 inches.
- All vital organs are mapped out and have begun to form.
- The heart has begun to develop valves and compartments.
- Tissue that develops into vertebrae forms, the brain develops into five areas and nerve cells are forming in the brain and spinal cord.
- The embryo responds to touch by reflex movements.
- Facial features - eyes, nose and mouth - continue to develop.
8 Weeks
 10 weeks after the first day of the last normal menstrual period.
10 weeks after the first day of the last normal menstrual period.
- The fetus, until now called an embryo, is about 1-1/4 to 1-1/2 inches long from head to rump (with the head making up about half this size) and weighs less than 1/2 ounce.
- All major organs and bodily systems are present, although few of them are functional.
- Muscles and skeleton are developing and movements are becoming purposeful.
- Structures that form eyes, ears, arms and legs are identifiable.
- Toes and eyelids begin to form.
10 Weeks
 12 weeks after the first day of the last normal menstrual period.
12 weeks after the first day of the last normal menstrual period.
- The fetus is about 2-1/2 inches from head to rump, weighing about 1-1/2 ounces.
- Fingernails and hair begin to develop and blood is formed in the liver.
- The fetus has distinct human characteristics.
- Sex can be identified.
- Urine formation begins.
12 Weeks
 14 weeks after the first day of the last normal menstrual period.
14 weeks after the first day of the last normal menstrual period.
- The fetus is about 3-1/2 inches from head to rump and weighs about 2 ounces.
- The fetus begins to swallow and the kidneys produce urine.
- Breathing movements are present.
- External genitals have been developing so that the sex can be identified.
- Bones are hardening in many locations.
- The nervous system is developing and the fetus may respond to skin stimulation.
- Taste buds cover the inside of the mouth.
2nd Trimester
14 Weeks
 16 weeks after the first day of the last normal menstrual period.
16 weeks after the first day of the last normal menstrual period.
- The fetus is about 4-3/4 to 5 inches from head to rump and weighs 4 ounces.
- The head is erect and the arms and legs are developed.
- The fetus can suck the thumb.
- Limb movements become more coordinated.
- If an ultrasound is performed at this time, the parents
- may be told the sex.
- The fetus has begun to kick, although the woman may not be able to feel the movement.
16 Weeks
 18 weeks after the first day of the last normal menstrual period.
18 weeks after the first day of the last normal menstrual period.
- The fetus is about 5 to 5-1/2 inches from head to rump and weighs 7 to 8 ounces.
- The skin is pink and transparent and the ears are clearly visible.
- The fetus can now suck, open the mouth and cover the face with the hands.
- Hair and nails begin to grow.
- The fetus can bend and flex the extremities, fingers, wrists, legs and toes and make breathing movements.
- Ovarian follicles are forming
- The brain has been rapidly growing and the central nervous system extends its connections from the brain to most parts of the body.
18 Weeks
 20 weeks after the first day of the last normal menstrual period.
20 weeks after the first day of the last normal menstrual period.
- The fetus is about 6-1/4 inches from head to rump, weighing about 10 to 12 ounces.
- All organs and structures have been formed, and a period of simple growth begins.
- The skin is covered with vernix - a greasy material that protects the skin.
- By this time, the woman may feel the fetus moving.
- Fingerprints are permanently established.
- Fine, downy hair covers the fetus.
20 Weeks
 22 weeks after the first day of the last normal menstrual period.
22 weeks after the first day of the last normal menstrual period.
- The fetus is about 7-1/2 inches from head to rump, weighing about one pound (16 ounces).
- Eyes are fully formed and eyebrows and eyelids are present.
- Head and body are covered with hair.
- Myelin insulation of the spinal cord, which increases the speed that nerves transmit impulses to the brain, is progressing.
- Pain receptors are present throughout the body and all physical structures necessary to feel pain are present.
- There is almost no chance that a fetus could survive outside the woman's body.
22 Weeks
 24 weeks after the first day of the last normal menstrual period.
24 weeks after the first day of the last normal menstrual period.
- The fetus is about 8 inches from head to rump and weighs about 1-1/4 pounds.
- The fetus hears sounds such as the woman's breathing, heartbeat and voice.
- Rapid eye movement begins, an activity associated with dreaming.
- The fetus is capable of hiccupping and grasping.
- Pain receptors are present throughout the body and all physical structures necessary to feel pain are present. Scientific studies have found that a human fetus does not have the capacity to experience pain until at least 24 weeks gestation.
- In rare cases, infants born as young as 22 weeks survive, but a high percentage have significant complications that affect their long-term survival.
Third Trimester
24 Weeks
 26 weeks after the first day of the last normal menstrual period.
26 weeks after the first day of the last normal menstrual period.
- The fetus is about 9 inches from head to rump and weighs about 2 pounds.
- Substantial weight gain occurs in this period and the fetus is better proportioned.
- Lungs produce a substance necessary for breathing after birth.
- Pain receptors are present throughout the body and all physical structures necessary to feel pain are present. Researchers disagree as to whether or not pain is perceived by the fetus.
- Infants born between 24 weeks and term have a good chance of survival with intensive medical care.
26 Weeks
 28 weeks after the first day of the last normal menstrual period.
28 weeks after the first day of the last normal menstrual period.
- The fetus is about 10 inches from head to rump and weighs about 2-1/2 pounds.
- The lids are now partially open.
- Most of the sense organs are now mature.
- Pain receptors are present throughout the body and all physical structures necessary to feel pain are present. Researchers disagree as to whether or not pain is perceived by the fetus.
- Most of the infants born now will survive (with intensive care services).
28 Weeks
 30 weeks after the first day of the last normal menstrual period.
30 weeks after the first day of the last normal menstrual period.
- The fetus is about 10-1/2 inches from head to rump and weighs almost 3 pounds.
- The fetus has lungs that are capable of breathing air, although intensive care may be needed.
- Rhythmic breathing and body temperature are now controlled by the brain (or Central Nervous System).
- Pain receptors are present throughout the body and all physical structures necessary to feel pain are present. Researchers disagree as to whether or not pain is perceived by the fetus.
- Nearly all infants born now will survive (with intensive care services).
30 Weeks
 32 weeks after the first day of the last normal menstrual period.
32 weeks after the first day of the last normal menstrual period.
- The fetus is about 11 inches from head to rump and weighs more than 3 pounds.
- Skin is thicker and pinker.
- Eyes respond to light.
- From this stage on, fetal development centers mostly around growth.
- It is generally agreed that the fetus perceives pain from 29 or 30 weeks, if not before.
- Almost all infants born now will survive (with intensive care services).
32 Weeks
 34 weeks after the first day of the last normal menstrual period.
34 weeks after the first day of the last normal menstrual period.
- The fetus is about 11-3/4 to 12 inches from head to rump and weighs about 4-1/2 pounds.
- The skin is now pink and smooth.
- Fingernails have reached fingertips.
- It is generally agreed that the fetus perceives pain from 29 or 30 weeks, if not before.
- Almost all infants born now will survive (some will need intensive care services).
34 Weeks
 36 weeks after the first day of the last normal menstrual period.
36 weeks after the first day of the last normal menstrual period.
- The fetus is about 12-1/2 inches from head to rump and weighs about 5-1/2 pounds.
- It is generally agreed that the fetus perceives pain from 29 or 30 weeks, if not before.
- Infants born at 33 weeks or more survive outside the womb, usually without medical help.
36 Weeks
 38 weeks after the first day of the last normal menstrual period.
38 weeks after the first day of the last normal menstrual period.
- The fetus is about 13-1/2 inches from head to rump and weighs about 6-1/2 pounds.
- Toenails have reached tips of toes.
- The fetus can grasp firmly.
- Fetus turns toward light sources.
- It is generally agreed that the fetus perceives pain from 29 to 30 weeks, if not before.
- Infants born at 33 weeks or more survive outside the womb, usually without medical help.
38 Weeks
 40 weeks after the first day of the last normal menstrual period.
40 weeks after the first day of the last normal menstrual period.
- The fetus is about 14 inches from head to rump, may be more than 20 inches overall and may weigh from 6-1/2 to 10 pounds.
- The fetus can now hear, taste, smell and feel.
- The fetus is full-term and ready to be born.
40 Weeks

Abortion Methods and Their Associated Medical Risks
If a woman has made an informed decision and chosen to have an abortion, she and her doctor must first determine how far her pregnancy has progressed. The gestational age of the embryo or fetus will directly affect the appropriateness or method of abortion.
Different methods of abortion are used at different gestational ages. Because the date of the beginning of the last normal period may be uncertain, women are advised to have an ultrasound exam to determine the gestational age of the embryo or fetus.
Abortion Risks
At or prior to eight weeks after the first day of the last normal menstrual period is considered the safest time to have an abortion. The risk of complications for the woman in- creases with advancing gestational age. The US Food and Drug Administration (FDA) states: "Although cramping and bleeding are an expected part of ending a pregnancy, rarely, serious and potentially life-threatening bleeding, infections, or other problems can occur following a miscarriage, surgical abortion, medical abortion, or childbirth."
Risks associated with early abortion, including death, are relatively low. Serious and minor complications following medical, aspiration or D & E abortions are also infrequent. Possible complications include infection, missed or incomplete abortion, cervical tear, uterine perforation and hemorrhage require transfusion. Minor complications are estimated to occur in fewer than 2.5% of abortions and serious complications (those requiring hospitalization) in fewer than .5%. Recently, increased risk of premature birth has been shown to be associated with abortion. Premature births are associated with infant mortality and childhood complications such as chronic lung disease, cerebral palsy, sensory deficits, cognitive impairments and behavior problems.
The risks or possible complications associated with an abortion are listed under each abortion procedure and are further described under the Medical Risks of Abortions and Long-Term Medical Risks sections.
Methods Used Prior to Fourteen Weeks
Early Non-Surgical Abortion
Non-surgical (medical) abortion is an abortion method approved by the FDA for pregnancies up to 70 days after the last menstrual period. This method is also referred to as RU-486.
- A drug is given that stops the hormones needed for the fetus to grow. The drug also causes the placenta to separate from the uterus, ending the pregnancy.
- A second drug is given by mouth or placed in the vagina causing the uterus to contract and push out the fetus and placenta, ending the pregnancy. An appropriate location should be selected for taking these drugs, because they may cause bleeding, cramps, nausea, diarrhea and other symptoms that usually begin within 2 to 24 hours.
- 7 to 14 days after taking the drugs, a woman must return to the doctor to make sure that the drugs succeeded in ending the pregnancy and that the fetus and placenta are completely gone from the uterus.
- If the pregnancy is not ended by the drug combination, a surgical abortion may be required.
Who should not have a non-surgical abortion?
According to the FDA, women should not use the drugs in a medical (non-surgical) abortion who:
- Are using an IUD (intrauterine device or system); it must be taken out before a medical abortion
- Have a pregnancy outside the uterus (ectopic pregnancy)
- Have problems with their adrenal glands (chronic adrenal failure)
- Take medication to thin their blood
- Have a bleeding problem
- Have porphyria
- Take certain steroid medicines
- Have allergies to either of the drugs used in the abortion method
- Ask your healthcare provider if you are not sure about all your medical conditions before taking these drugs.
Possible Complications or Adverse Events
Cramping and vaginal bleeding are expected with this abortion. The complication rate for first trimester non-surgical abortion is 5% (four times the complication rate of aspiration abortion).
Rarely, serious and potentially life-threatening complications occur:
- Heavy bleeding (hemorrhage)
- Infections
- Incomplete abortion
The most common side effects are:
- Nausea and/or vomiting
- Weakness
- Diarrhea
- Fever/chills
- Dizziness
- Headache
Vacuum Aspiration Abortion
Vacuum aspiration is the most common used method of induced abortion in the United States.
- A local anesthetic is applied or injected into or near the cervix to reduce discomfort or pain.
- The opening of the cervix is gradually stretched with a series of dilators. The thickest dilator used is about ½ inch wide.
- A cannula (a thin, hollow tube with a sharp pointed end) is inserted into the uterus.
- The cannula is attached to a suction system that removes the fetus, placenta and membranes from the woman's uterus.
- A follow-up appointment should be made with the doctor.
Possible Complications or Adverse Events
Cramping and vaginal bleeding are an expected part of this abortion. The overall complication rate for vacuum aspiration abortion is approximately 1.25%.
Complications include:
- Incomplete abortion
- Infection
- Heavy bleeding (hemorrhage)
- Torn cervix
- Perforated uterus
- Premature birth associated with subsequent pregnancies
- Rarely, serious and life-threatening complications occur
Methods Used After Fourteen Weeks
Dilatation and Evacuation (D&E)
- The cervix is dilated using one of the following methods. One method uses sponge- like tapered pieces of absorbent material laced into the cervix to dilate the cervix over a period of several hours or overnight. Another method is to insert dilating rods of increasing sizes in the cervix until the cervix has been dilated to an opening wide enough to accept the medical instruments.
- Following dilation of the cervix, intravenous medications may be given to ease discomfort or pain and prevent infection.
- After a local or general anesthesia has been administered, the fetus and placenta are removed from the uterus with medical instruments such as forceps and suction. Occasionally for removal, it may be necessary to dismember the fetus.
Possible Complications or Adverse Events
Cramping and vaginal bleeding are an expected part of this abortion.
- Blood clots in the uterus
- Heavy bleeding
- Cut or torn cervix
- Perforation of the wall of the uterus
- Pelvic infection
- Incomplete abortion
- Anesthesia-related complications
- Rarely, death
Labor Induction (Including Intra-Uterine Instillation)
- Labor induction may require a hospital stay.
- Medicine is placed in the cervix to soften and dilate it.
- There are three ways to start labor early:
- Medication is given directly into the bloodstream (vein) of the pregnant woman to start uterine contractions.
- Medication inserted into the vagina to start uterine contractions.
- Medication is injected directly into the amniotic sac by inserting a needle through the woman's abdomen and into the amniotic sac (bag of waters). This medication kills the fetus and starts uterine contractions.
- Labor and delivery of the fetus during this period are similar to the experiences of childbirth.
- The duration of labor depends on the size of the fetus and the contractility of the uterus.
- There is a small chance that a fetus could live for a short period of time depending on the fetus's gestational age and health at the time of delivery.
Possible Complications
- This method is more physically and emotionally stressful to the woman than the D&E method.
- If the placenta is not completely removed during labor induction, the doctor must open the cervix and use suction aspiration to remove remaining placenta and tissue.
- Labor induction abortion carries the highest risk for problems, such as infection and heavy bleeding.
- When medicines are used to start labor, there is a risk of rupture of the uterus.
- As with childbirth, possible complications of labor induction include infection, heavy bleeding, stroke and high blood pressure.
- Other medical risks may include blood clots in the uterus, heavy bleeding, cut or torn cervix, perforation of the wall of the uterus, pelvic infection, incomplete abortion, and anesthesia related complications.
Medical Risks of Abortion
The risk of complications for the woman increases with advancing gestational age (see above for a description of the abortion procedure that your doctor will be using and the specific risks). Medical abortions have four times as many complications as surgical abortions.
Pelvic Infection (Sepsis): Bacteria (germs) from the vagina may enter the cervix and uterus and cause an infection, blood can become infected (septicemia), surgical incisions can become infected and infections from unknown sources can develop. Infections can be mild or severe. Antibiotics are used to treat an infection. In rare cases, a repeat suction, hospitalization or surgery may be needed. Infection rates are about .2% for first trimester medical and surgical abortions and under 1% for dilation and evacuation (D & E), and 5% for labor induction.
Incomplete Abortion: Fetal parts or other products of pregnancy may not be completely emptied from the uterus, requiring further medical procedures. Incomplete abortion may result in infection and bleeding. In the first trimester, the reported rate of such complications is between 5% and 10% for medical abortions and less than 1% after a dilation and curettage (D & C). In later abortions, the rate is less than 1% in dilation and evacuation (D & E) following a labor induction procedure, the rate may be as high as 36%.
Blood Clots in the Uterus: Blood clots that cause severe cramping occur in about 1% of all abortions. The clots usually are removed by a repeat dilation and suction curettage.
Heavy Bleeding (Hemorrhage): Some amount of bleeding is common following an abortion. Heavy bleeding (hemorrhaging) is not common and may be treated by repeat suction, medication or, rarely, surgery. Ask the doctor to explain heavy bleeding and what to do if it occurs.
Cut or Torn Cervix: The opening of the uterus (cervix) may be torn while it is being stretched open to allow medical instruments to pass through and into the uterus. This happens in less than 1% of first trimester abortions.
Perforation of the Uterus Wall: A medical instrument may go through the wall of the uterus. The reported rate is 1 out of every 1,000 with early abortions and 3 out of every 1,000 with dilation and evacuation (D & E). Depending on the severity, perforation can lead to infection, heavy bleeding or both. Surgery may be required to repair the uterine tissue, and in the most severe cases hysterectomy may be required.
Anesthesia-Related Complications: As with other surgical procedures, anesthesia increases the risk of complications associated with abortion. The reported risks of anesthesia- related complications is around 1 per 5,000 abortions. Most are allergic reactions producing fever, rash and discomfort.
Long-Term Medical Risks
Future childbearing: Early abortions that are not complicated by infection do not cause infertility. Complications associated with an abortion may make it difficult to become pregnant in the future or carry a pregnancy to term.
Premature Birth: Increased risk of premature birth has been shown to be associated with abortion. Premature babies ("preemies") have higher risk of death in their first year of life and raised risk of autism, cerebral palsy, deafness, blindness, and cognitive impairments (developmental disability).
Cancer of the Breast: The National Cancer Institute (NCI) and the American Cancer Society (ACS) report that scientific research studies have shown no increased risk of developing breast cancer if a woman has had an abortion.
Medical Emergencies
When a medical emergency requires the performance of an abortion, the physician shall tell the woman, before the abortion if possible, of the medical indications supporting the physician's judgment that an abortion is necessary to avert her death or that a 24-hour delay will create serious risk of substantial and permanent impairment of a major bodily function.
Fetal Pain
There is no evidence to suggest that a fetus experiences pain. According to the American College of Obstetricians and Gynecologists, scientific studies have found that a human fetus does not have the capacity to experience pain until at least 24 weeks gestation.
The Emotional Side of Abortion
Feelings and Emotions
Stress and anxiety is expected when making a decision about a pregnancy---whether deciding to continue the pregnancy, have an abortion, or place the child for adoption. These feelings are normal. Some women may experience loss of appetite, difficulty sleeping and loss of interest in enjoyable activities. Reaching out to family and friends can provide essential support during this time. If these feelings continue or get worse, you should contact your health care provider.
Talk It Over
Talking with a counselor or physician not associated with an abortion provider may help a woman to consider her decision fully before taking any action. Many organizations listed in the Minnesota Department of Health Resource Guide offer counseling services at no cost. The directory is online: If You Are Pregnant: A Directory of Services Available in Minnesota.
The Medical Risks of Childbirth
Labor is the process in which a woman's uterus contracts and pushes, or delivers, the fetus from her body. The fetus may be delivered through the woman's vagina, or by caesarean section. A caesarean section is a surgical procedure that delivers the fetus after making a cut (incision) through the woman's belly and uterus.
A woman who carries the pregnancy to full term (40 menstrual weeks, 38 weeks after fertilization) can usually expect to experience a safe and healthy process. For a woman's best health, she should visit her physician before becoming pregnant, early in her pregnancy, and at regular intervals throughout her pregnancy.
Possible Complications
- Uterine infection – 10% may develop during or after delivery, and on rare occasions cause death
- Blood pressure problems – 1 in 20 pregnant women have during or after pregnancy, especially first pregnancies
- Blood loss – 1 in 20 women experience during delivery
- Rare events such as blood clot, stroke or anesthesia – related death
- Women with severe chronic diseases are at greater risk of developing complications during pregnancy, labor and delivery
- Risk of dying as the result of a pregnancy complication is 12 per 100,000 women
Resources for Women with Adverse Pregnancy Diagnoses
Sometimes prenatal testing or screening reveals an unexpected diagnosis of a serious disease, deformity or chromosomal disorder. Initial fear or medical care providers may lead a woman toward abortion. In these circumstances, a woman may want to get a second opinion due to the possibility of false positive test results. Perhaps she may simply want to get additional information before making a decision. Connecting with other parents who have children with the same or a similar condition has the ability to bring comfort and a new perspective. This connection with those who have knowledge of the benefits of medical care and useful therapies, support groups, and the everyday realities of caring for their children, allows a woman to see beyond the diagnosis and consider parenting her child or placing her child for adoption in a family she may feel is better able to provide for his or her needs.
Prenatal Partners for Life - This Minnesota organization provides support, information and encouragement for women and families with an adverse prenatal diagnosis, as well as support for raising children with special needs after birth.
SOFT (Support Organization for Trisomy) - SOFT is a valuable resource for patients and families seeking information about support and medical subjects. Resources include a free e-booklet "Care of the Infant and Child with Trisomy 18 or Trisomy 13".
International Trisomy Alliance - ITA offers trisomy 13 and trisomy 18 support groups, physicians and other professionals' accurate information and resources. Resources include booklet "Preparing for your Baby's Arrival".
Down Syndrome Association of Minnesota - This organization provides information and support to people with Down syndrome, their families and communities. Their website includes an Expectant Parent page and a New Parent page.
National Down Syndrome Adoption Network - The mission of this organization is to ensure that every child born with Down syndrome has the opportunity to grow up in a loving family. There are no fees for any of the services of the NDSAN.
Down Syndrome Diagnosis Network - Provides resources, education and support to women and families who receive a diagnosis of Down syndrome; makes connections to other parents with Down syndrome (trisomy 21) children.
Financial Assistance for Pregnancy, Childbirth, and Newborn Care
You may qualify for financial help for prenatal (pregnancy), childbirth and neonatal (newborn) care, depending on your income. For people who qualify, programs such as Medical Assistance (MA) or MinnesotaCare may pay or help pay the cost of doctor, clinic, hospital and other related medical expenses to help with prenatal care, childbirth delivery services and care for newborns. You can apply for health coverage by going to MNSure. Click on 'Medical Assistance or MinnesotaCare' or 'special enrollment period'. Being pregnant qualifies you for special enrollment as a life event. You can also call MNSure at 855-366-7873.
Adoption as an Option
Women or couples facing an untimely pregnancy may choose to make an adoption plan.
Counseling and support services are key parts of the adoption decision process. These resources are available from a number of public and private adoption agencies without obligation or commitment. All adoption services are available to birthparents without cost. Further information and a list of adoption agencies can be found in the Minnesota Department of Health resource guide, If You Are Pregnant: A Directory of Services Available in Minnesota.
There are several ways to consent to the adoption of a child. Talking with a Minnesota Licensed Adoption Agency or an attorney familiar with adoption will help identify the method that will best serve you and your baby. Birth parents decide whether they want to remain anonymous or participate in a more open adoption that includes selecting adoptive parents and establishing a plan for communication over time.
Minnesota Safe Haven Law
After your baby is born, if you are unable or unwilling to care for him or her, you can take your baby to any licensed hospital in Minnesota and give him or her to a hospital employee. You can do this until the baby is three days old, no questions asked. You are not required to give your name or any other information. It's safe and anonymous. You do not need to tell anyone. If you would rather not go yourself, you can give a family member, friend or any responsible adult permission to bring your baby to a hospital.
For more information, go to Safe Haven
The Father's Responsibility
The father of a child has a legal responsibility to provide for the financial support, medical care and other needs of his child. In Minnesota, that responsibility includes child support payments to the child's mother or legal guardian. Children have rights of inheritance from their father and may be eligible through him for benefits such as life insurance, Social Security, pension, veteran's or disability benefits. Additionally, children benefit from knowing their father's medical history and any potential health problems that can be passed genetically.
Paternity can be established in Minnesota by:
- Recognition of Parentage: The biological parents state under oath that they are the parents of the child. This statement will assure benefits to the child. It also will establish the father's parental rights.
- Adjudication: A legal action can be brought in court to determine the biological and legal father of a minor child. This process, in addition to obtaining all of the benefits of a Recognition of Parentage, establishes child support orders, custody and visitation rights. An adjudication also establishes paternity when paternity is contested. It provides legal safeguards to all parties involved.
Issues of paternity affect the legal rights of both parents and of the child. You can get general information about paternity establishment, federal regulations and state statutes about child support, and related issues 24 hours a day, seven days a week by calling:
651-431-4199 (General Information Line)
Or you can write to:
Minnesota Department of Human Services Child Support Enforcement Division
P.O. Box 64946
St. Paul, MN 55164-0946
Information Directory
The decision to have an abortion, have a baby or make an adoption plan must be carefully considered. There are lists of state, county and local health and social service agencies and organizations available to assist you. You are encouraged to contact these groups if you need more information so you can make an informed decision.
You can find what resources may be available to you in the Minnesota Department of Health resource guide, If You Are Pregnant: A Directory of Services Available in Minnesota or you can call 651-201-3580 or 1-888-234-1137.
How Do People Not Know They Are Pregnant Domain_10
Source: https://www.health.state.mn.us/people/wrtk/handbook.html
0 Response to "How Do People Not Know They Are Pregnant Domain_10"
Post a Comment